St Andrew's Healthcare calls on the Government to prioritise complex mental health

We are calling on the NHS to help “break the stigma” commonly associated within the health sector.
St Andrew’s Healthcare has been consulting with staff, patients and carers, about what they want to see included in the NHS Long Term Plan. Due for publication next spring, it will outline what the priorities will be for the health service over the next 10 years.
As part of the consultation, launched by the Health Secretary at the end of October, St Andrew’s, Executive Medical Director, DR Sanjith Kamath, has set out what the charity would like the NHS to consider.
Dr Kamath said: “When it comes to understanding mental health we’ve come a long way. But, if we’re talking about complex mental health, we still have a lot of work to do.
“There’s often fear of people who have serious mental illness. We only have to look at how people with complex mental health problems are portrayed in films, rarely are they shown in a good light. Other media also tend to emphasise how individuals with mental illness can be dangerous. But, actually there is evidence to suggest that individuals with serious mental illness are much more likely to be a victim of a crime than a perpetrator.
“We need to overcome the barrier of stigma and educate society that people with these conditions should not be judged, but instead should be supported by their community. In order for this to happen though, we must change public perceptions of complex mental illness and ensure communities and services are equipped to support vulnerable people with dignity and compassion.”
Dr Kamath has also highlighted the large number of people currently residing in hospital who are well enough to move on, but are unable to do because there is not a suitable community placement for them. In fact, recent analysis shows there are more than 3,000 people across the country who are stuck in mental health hospitals when they no longer have a medical need to be there.
He said: “People cannot live their lives in hospital. That’s why, as part of our response to the NHS long-term plan, we are calling on the Government to help individuals with complex mental illness live independently. In order for this to happen, we need better training, better housing support, and much better community services.”
It is hoped the reform of the Mental Health Bill, which is currently progressing through parliament, will modernise the sector’s approach to mental health.
Dr Kamath added: “Once the bill passes, each patient will legally be entitled to have care and treatment plans which will clearly describe what is needed to progress them to discharge, but without the community placements, I’m not sure how this will happen.”
St Andrew’s has already started with this approach as part of the National Transforming Care programme. Earlier this year, a bespoke Supported Transition Service was opened within its Northampton grounds. This means patients, who have very complex and specific needs, can live more independently outside a ward environment, with trained staff on standby to support the individual when needed.
Lime Tree Cottage is a single occupancy hospital-registered house that supports active rehabilitation and independent community skill development, all wrapped up within a safe environment.
Dr Kamath said: “Lime Tree has already been a huge success and we’ve had positive feedback from the patient who resides there, and his family. This is a model of care we’re planning on replicating as it is very important to us that when our patients are ready to move on, we have an appropriate placement for them.”
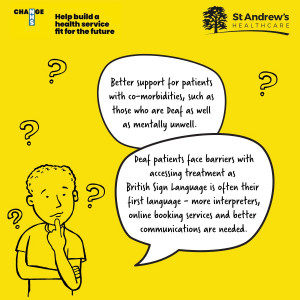
The general consensus among staff and patients, who were asked to consider what else they would like the NHS to focus on in the future, was prevention.
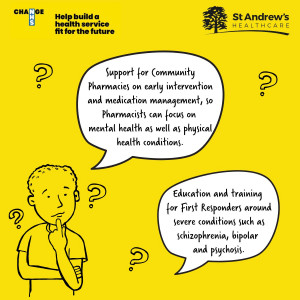
Dr Kamath added: “We’re all aware of the old adage that prevention is better than cure. The same can also be applied to early intervention. We’re advocating for universal mental health screenings and more training for GPs and emergency responders, so they have an even better understanding of conditions such as schizophrenia, bipolar and psychosis.
“We also want to see a real focus on improving physical health outcomes for people living with severe mental illness as evidence suggests they tend to die 20 years earlier than those without.
“At St Andrew’s we are already playing a part in that as our Lightbulb Mental Wellness Programme for Schools, gives teachers, carers and children the tools to recognise symptoms early and know when and who to ask for help.”
Thank you to all colleagues, patients and carers who shared their views as part of the consultation.
 PICU and Acute Bed Availability
PICU and Acute Bed Availability